The London Marathon is one of the highlights of the sporting calendar, and a showcase for the capital. Each spring,...
S Charlton
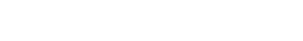
Plantar Fascia Release - Birmingham
I had a plantar fascia release to my left foot in August 2006. I had been suffering constant pain for 2 years prior to my surgery. I would like to let all at the Clinic know I no longer experience any pain from my left heel, despite being on my feet all day.